Physical therapy plays a crucial role in wound care by promoting healing, preventing complications, and improving overall function. Physical therapists work closely with wound care teams to develop individualized treatment plans that address the specific needs of each patient. They may use various techniques such as manual therapy, therapeutic exercises, and modalities like ultrasound or electrical stimulation to promote tissue healing, reduce pain, and improve range of motion. Additionally, physical therapists educate patients on proper wound care techniques, body mechanics, and strategies to prevent further injury or infection.
Rehabilitation ExercisesPhysical therapy can significantly aid in wound healing and prevent complications by addressing underlying factors that may impede the healing process. Through therapeutic exercises, physical therapists can improve circulation, which is essential for delivering oxygen and nutrients to the wound site. They can also help strengthen the surrounding muscles to provide support and stability, reducing the risk of further injury or pressure ulcers. Furthermore, physical therapists can assess and address any postural or gait abnormalities that may contribute to excessive pressure or friction on the wound, thus minimizing the risk of complications.
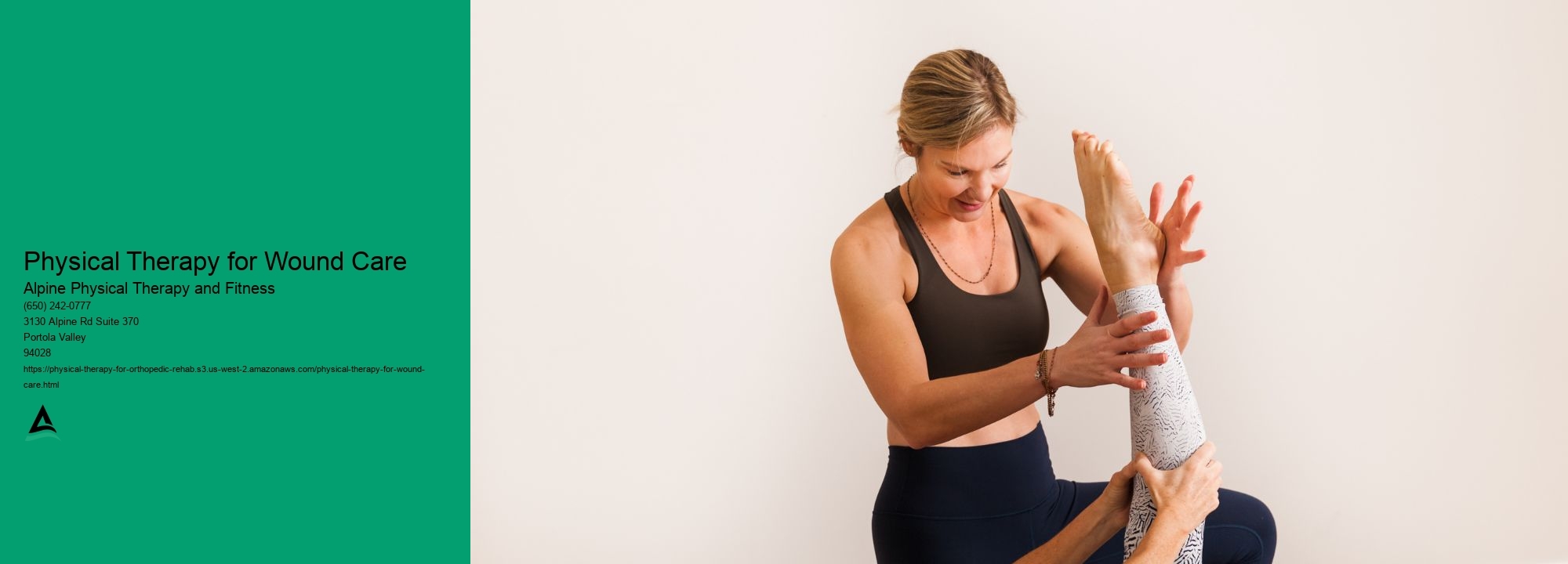
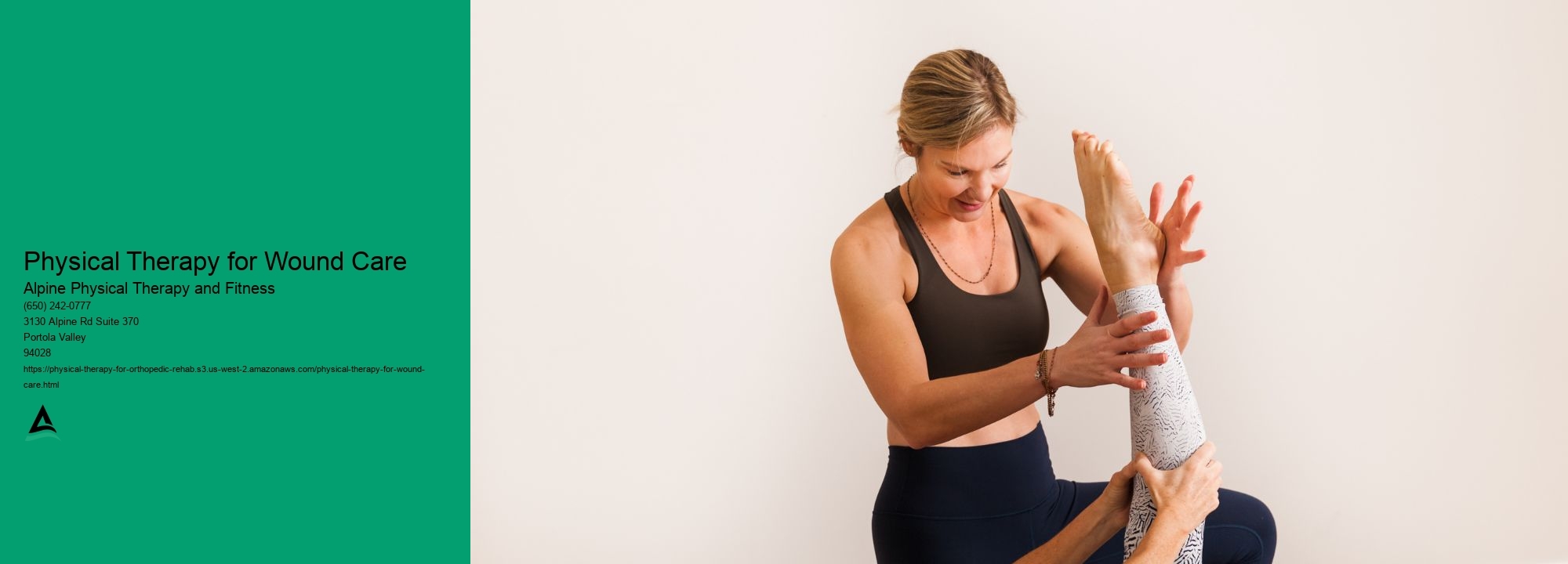
In physical therapy for wound care, specific exercises and techniques are employed to promote healing and improve function. These may include range of motion exercises to maintain joint mobility, strengthening exercises to improve muscle support around the wound, and stretching exercises to prevent contractures. Physical therapists may also use manual therapy techniques such as massage or scar tissue mobilization to improve tissue flexibility and promote proper healing. Additionally, they may incorporate modalities like heat or cold therapy, electrical stimulation, or ultrasound to enhance the healing process.
Yes, physical therapy can help with pain management during wound healing. Physical therapists are trained to assess and address pain associated with wounds. Orthopedic Bracing They may use various techniques such as manual therapy, therapeutic exercises, and modalities to reduce pain and improve overall comfort. Additionally, physical therapists can educate patients on proper positioning, body mechanics, and pain management strategies to minimize discomfort during wound healing.
While physical therapy is generally beneficial for wound care, there are some precautions and contraindications to consider. For example, if a wound is infected or has not yet been properly assessed by a healthcare professional, physical therapy may need to be delayed until the wound is appropriately managed. Pain Relief Modalities Additionally, certain medical conditions or medications may affect the healing process or increase the risk of complications, requiring modifications to the physical therapy treatment plan. It is essential for physical therapists to collaborate closely with the wound care team and consider the individual needs and circumstances of each patient.
The duration of physical therapy for wound care patients can vary depending on the severity and complexity of the wound, as well as the individual's response to treatment. In some cases, a few sessions may be sufficient to address specific issues and provide education on wound care and prevention. Rehabilitation Equipment However, for more complex wounds or patients with underlying conditions, a longer course of physical therapy may be necessary to achieve optimal healing and functional outcomes. The physical therapist will work closely with the patient and the wound care team to determine the appropriate duration of treatment.
Incorporating physical therapy into a wound care treatment plan offers several potential benefits. Arthritis Management Firstly, physical therapy can help optimize wound healing by promoting circulation, reducing inflammation, and improving tissue flexibility. Secondly, physical therapists can address any underlying musculoskeletal issues that may impede the healing process or contribute to complications. Thirdly, physical therapy can help patients regain or improve their functional abilities, enhancing their overall quality of life. Lastly, physical therapists can educate patients on proper wound care techniques, body mechanics, and strategies to prevent future wounds, empowering them to take an active role in their own healing and prevention journey.
Yes, there are specific protocols for rehabbing a scaphoid fracture. The rehabilitation process typically involves a combination of immobilization, physical therapy, and gradual return to normal activities. Immobilization is usually achieved through the use of a cast or splint to keep the wrist and hand stable and prevent further injury. Physical therapy may include exercises to improve range of motion, strength, and flexibility in the wrist and hand. This may include gentle stretching, strengthening exercises, and functional activities to help regain normal function. Gradual return to normal activities is important to ensure that the scaphoid fracture has fully healed and to prevent re-injury. It is important to follow the specific protocols and guidelines provided by a healthcare professional to ensure a safe and effective rehabilitation process.
Physical therapy can be highly beneficial in the rehabilitation of lateral epicondylitis, commonly known as tennis elbow. This condition is characterized by pain and inflammation on the outer part of the elbow, typically caused by repetitive motions of the forearm and wrist. Physical therapy interventions for tennis elbow may include a combination of exercises, manual therapy techniques, and modalities such as ultrasound or electrical stimulation. These interventions aim to reduce pain, improve range of motion, strengthen the affected muscles, and promote healing. Additionally, physical therapists may provide education on proper ergonomics and body mechanics to prevent further injury. Overall, physical therapy can play a crucial role in the successful recovery and functional restoration of individuals with lateral epicondylitis.
Physical therapy can be an effective treatment option for individuals experiencing post-fusion spine mobility issues. By utilizing a combination of targeted exercises, manual therapy techniques, and specialized equipment, physical therapists can help improve range of motion, reduce pain, and enhance overall function in the spine. Specific exercises may include stretching, strengthening, and stabilization exercises, as well as activities to improve posture and body mechanics. Additionally, physical therapists may employ modalities such as heat or cold therapy, electrical stimulation, or ultrasound to further enhance the healing process. Through a comprehensive and individualized treatment plan, physical therapy can play a crucial role in restoring mobility and optimizing outcomes for individuals who have undergone spinal fusion surgery.
Yes, there are several specialized stretches that can be effective in treating iliotibial band syndrome. These stretches target the iliotibial band, a thick band of connective tissue that runs along the outside of the thigh from the hip to the knee. Some of the recommended stretches include the standing IT band stretch, where the individual stands with one leg crossed over the other and leans to the opposite side, feeling a stretch along the outer thigh. Another effective stretch is the foam rolling technique, where the individual lies on their side and rolls a foam roller along the length of the iliotibial band, applying pressure to release tension. Additionally, the seated IT band stretch, where the individual sits with one leg straight and the other leg crossed over it, gently pulling the knee towards the opposite shoulder, can also help alleviate symptoms of iliotibial band syndrome. It is important to consult with a healthcare professional or physical therapist to ensure proper technique and to determine the most appropriate stretches for individual needs.
Physical therapy plays a crucial role in the comprehensive treatment of complex regional pain syndrome (CRPS). The primary goal of physical therapy in CRPS management is to alleviate pain, improve function, and enhance the overall quality of life for individuals suffering from this condition. Physical therapists employ a variety of techniques and modalities, such as manual therapy, therapeutic exercises, and neuromuscular re-education, to address the specific needs of each patient. These interventions aim to reduce pain, restore joint mobility, improve muscle strength and coordination, and promote overall physical well-being. Additionally, physical therapists may also incorporate other modalities like heat or cold therapy, electrical stimulation, and hydrotherapy to further enhance the effectiveness of treatment. By tailoring treatment plans to the individual needs of each patient, physical therapy can significantly contribute to the management and rehabilitation of individuals with CRPS.
Physical therapy plays a crucial role in rehabilitating a PCL tear by employing a comprehensive and individualized treatment plan. The therapist will focus on restoring knee stability, improving range of motion, and strengthening the surrounding muscles. This may involve a combination of exercises such as quadriceps sets, hamstring curls, and calf raises to enhance muscle strength and balance. Additionally, the therapist may incorporate modalities like ultrasound or electrical stimulation to reduce pain and inflammation. Manual therapy techniques, including joint mobilizations and soft tissue mobilizations, can help improve joint mobility and reduce scar tissue formation. The therapist may also provide education on proper body mechanics and functional training to ensure a safe return to daily activities and sports. By addressing the specific needs of the patient, physical therapy can effectively aid in the rehabilitation of a PCL tear, promoting optimal recovery and preventing future injuries.